Development Of Nursing Care Instruments Based On The 3s Framework (Sdki, Slki, Siki) For Inpatient Settings
DOI:
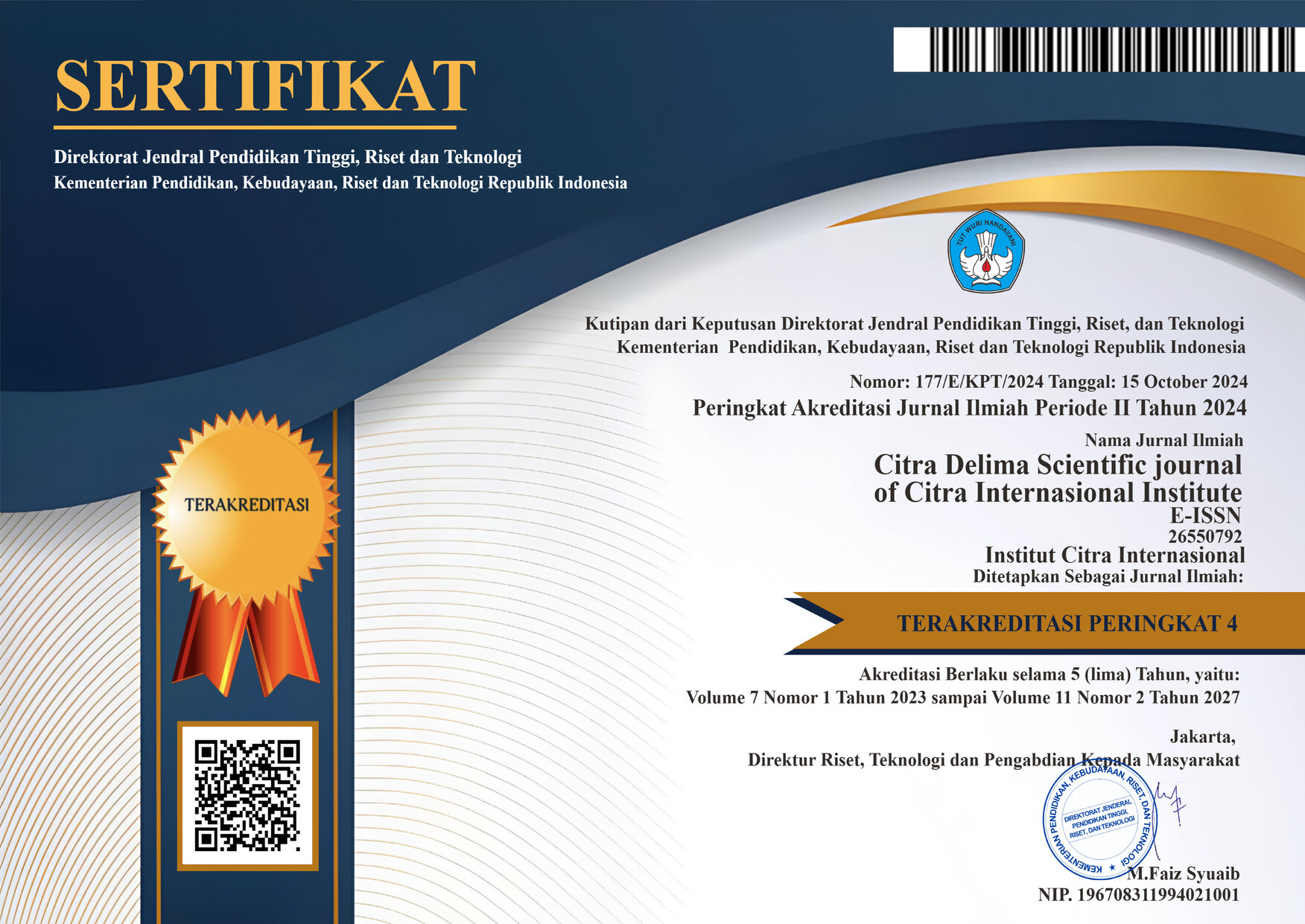
https://doi.org/10.33862/citradelima.v9i1.582Keywords:
Inpatient Settings, Instrument Development, Nursing Care Instrument, Nursing Documentation, Framework (SDKI, SLKI, SIKI)Abstract
Standardized nursing documentation is essential for ensuring consistency, accountability, and quality in patient care. In Indonesia, the 3S framework—comprising the Standar Diagnosa Keperawatan Indonesia (SDKI), Standar Luaran Keperawatan Indonesia (SLKI), and Standar Intervensi Keperawatan Indonesia (SIKI) serves as a national standard. However, its application in inpatient settings remains inconsistent due to the lack of integrated, user-friendly tools. This study aimed to develop and validate a nursing care documentation instrument based on the 3S framework to improve documentation accuracy, support clinical decision-making, and promote standardization in inpatient wards. A Research and Development (R&D) approach was employed, using a modified Borg and Gall model across five stages: preliminary study, planning, product development, expert validation, and limited field testing. Data were gathered through literature reviews, chart audits, clinical interviews, and focus group discussions with nurses. The instrument was designed to address the 12 most frequently encountered nursing diagnoses in general medical-surgical wards, which were systematically mapped to appropriate SLKI outcomes and SIKI interventions. The final tool features structured diagnosis formats (PES, PR, PS), outcome targets with timelines, and categorized interventions (observation, treatment, education, collaboration), implemented in a shift-based checklist format. Validation by five expert nurses yielded strong content validity (I-CVI range: 0.833–1.000), and field testing with 15 clinical nurses demonstrated acceptable internal consistency (KR-20: 0.790–0.845). Additionally, 87% of nurses reported improvements in documentation quality and workflow efficiency. In conclusion, the 3S-based nursing care instrument is valid, reliable, and practical for clinical use, and its adoption is recommended to enhance nursing documentation standards and the quality of care in hospital settings.
Downloads
References
Abd El Rahman, A., Ibrahim, M., & Diab, G. (2021). Quality of Nursing Documentation; progress notes in damage evaluation and its impact on Continuity of patient care. Menoufia Nursing Journal, 6(2), 1–18. https://doi.org/10.21608/menj.2021.206094
Ackley, B. J. (2024). Nursing Diagnosis Handbook; An Evidence-Based Guide to Planning Care-12th Edition Revised Reprint with 2021-2023 NANDA (M. Z. Betty J. Ackley, Gail B. Ladwig, Mary Beth Flynn Makic, Marina Reyna Martinez-Kratz (ed.); 12th ed., pp. 267–284). Elsevier
Alligood, M. R. (2022). Nursing Theorists (Tenth, pp. 251–278). Elsevier Health Sciences. https://doi.org/https://www.google.co.id/books/edition/Nursing_Theorists_and_Their_Work_E_Book/usg5EAAAQBAJ?hl=id&gbpv=1
Amir, H., & Kaseger, H. (2023). Pengaruh Pelatihan Pedoman Standar Diagnosis Keperawatan Indonesia (SDKI) Terhadap Sistem Pemberian Asuhan Keperawatan di Puskesmas Kabupaten Bolaang Mongondow. PREPOTIF Jurnal Kesehatan Masyarakat, 7, 16049–16054
Berman, A., Frandsen, G., & Snyder, S. (2021). Kozier & Erb’s Fundamentals of Nursing?; Concepts, Process and Practice (S. J. Snyder & G. Frandsen (eds.); Tenth, pp. 455–461). Julie Levin Alexander
Cuda, S. E., & Censani, M. (2022). Assessment, Differential Diagnosis, and Initial Clinical Evaluation of The Pediatric Patient with Obesity: An Obesity Medical Association (OMA) Clinical Practice Statement 2022. Obesity Pillars, 1(January), 1–6. https://doi.org/10.1016/j.obpill.2022.100010
Doengoes, M. E., & Moorhouse, M. F. (2019). Nursing Care Plans; Guidelines For Individualizing Client Care Across The Life Span (A. C. Murr (ed.); 10th ed., pp. 331–369). F.A Davis Company
Harding, M., & Hagler, D. (2022). Conceptual Nursing Care Planning (L. Newton (ed.); pp. 325–343). Book Aid International
Haugen, N. (2022). Nursing Care Planning; Prioritization, DElegation, and Clinical Reasoning. Revised Reprint With 2021-2023 NANDA-I (S. J. Galura (ed.); 8th ed., pp. 368–411)
Hidayat, A. A. (2021). Nursing Process NANDA, NIC, NOC, and SDKI Approaches (N. A. Aziz (ed.); Pertama, pp. 105–122)
Hockendberry, M. J. (2020). Wong’s: Nursing Care of Infants and Children; 11th Edition. In D. Wilson (Ed.), American Speech (11th ed., Vol. 15, Issue 3). Elsevier Health Sciences. https://doi.org/10.2307/486972
Jannah, N. (2020). Nursing Care Documentation Standards and Models. 9. https://doi.org/https://osf.io/nh8yd
Kamil, H., Rachmah, R., Wardani, E., & Björvell, C. (2020). How to optimize integrated patient progress notes: A multidisciplinary focus group study in Indonesia. Journal of Multidisciplinary Healthcare, 13, 1–8. https://doi.org/10.2147/JMDH.S229907
Kartini, M., & Eka Ratnawati. (2022). The Effectiveness of Nursing Documentation Training on Nurse’s Knowledge about SDKI, SLKI, and SIKI). Jurnal Kesehatan, 11(1), 47–51. https://doi.org/10.46815/jk.v11i1.78
Mayenti, F., Meri, D., & Maria, L. (2024). Sosialisasi Pendokumentasian Asuhan Keperawatan Berbasis SDKI, SLKI dan SIKI di RS Sansani Pekanbaru. Jurnal Abdimas Kesehatan (JAK), 6(1), 119. https://doi.org/10.36565/jak.v6i1.676
Ministry of Health Republic Indonesia. (2023). Main Results of Basic Health Research. Kementrian Kesehatan RI. https://doi.org/https://kemkes.go.id/eng/home
Muharni, S. (2024). Introduction to 3S (SDKI, SLKI, SIKI) in Documenting Nursing Care. Jurnal Abdidas, 2(5), 1092–1098. https://doi.org/http://abdidas.org/index.php/abdidas Persiapan
Murtiningsih, Zaly, N. wati, Wulandari, D. F., & Suhendry, A. (2021). Pelatihan Asuhan Keperawatan Spiritual Menggunakan Buku Panduan Persatuan Perawat Nasional Indonesia melalui Teleconference Bagi Perawat dan Bidan RSUD Depok. Kesehatan Dan Kedokteran, 5(2), 33–38.
https://doi.org/http://journal.fdi.or.id/index.php/jatiemas/article/view/423/268
Muzaenah, T., Yulistiani, M., Nurjanah, S., & Istianah. (2023). In House Training Upaya Peningkatan Kemampuan Perawat Dalam Memenuhi Kebutuhan Spiritual Care Pasien. Jurnal Inovasi Dan Pengabdian Masyarakat Indonesia, 2(1), 9–13. https://doi.org/10.26714/jipmi.v2i1.72
Nahak, M. P. M. (2023). The Effectiveness of Nursing Documentation Training Using Technical Guideline on Nursing Documentation skills in Nursing Students at Universitas Timor. Jurnal Ilmiah Keperawatan (Scientific Journal of Nursing), 9(1), 130–139. https://doi.org/10.33023/jikep.v9i1.1388
Polit, D., & Beck, C. (2019). Nursing Research (11th ed., pp. 284–304). Philadelphia: Wolters Kluwer Health
Potter and Perry. (2021). Fundamentals of Nursing: Second South Asia Edition (S. K. Sharma (ed.); Third Sout, pp. 537–576). Elsevier, RELX India Pvt. Ltd
Purnamasari, I., Raharyani, A. E., & Karim, Y. (2023). In House Training 3S (SDKI. SLKI, SIKI) to Improve Nurses’ Knowledge of 3S-Based Nursing Care. Indonesian Journal of Global Health Research, 5(1), 35–42. https://doi.org/10.37287/ijghr.v5i1.1482
Rendana, A., & Muharni, S. (2023). Pengaruh Pelatihan 3 S (SDKI, SIKI, SLKI) Terhadap Pengetahuan Perawat Dalam Pendokumentasian Asuhan Keperawatan. Jurnal Ilmiah Ilmu Keperawatan, 14(2), 34–45. https://doi.org/10.52395/ujpkm.v2i1.332
Sari, N. K., Prihatiningsih, T. S., & Lusmilasari, L. (2021). Key elements of professional nursing practice: A scoping review. Open Access Macedonian Journal of Medical Sciences, 9(T4), 253–260. https://doi.org/10.3889/oamjms.2021.5885
Sege, M., Dedi, B., & Tukayo, I. J. H. (2022). The Influence of the Design of Nursing Care Documentation Design SDKI, SLKI, SIKI (3S) in Hospital Management Information Systems on Nurse Satisfaction at Dian Harapan Jayapura Hospital. Journal of Social Science, 3(6), 2073–2080. https://doi.org/10.46799/jss.v3i6.436
Sulistyawati, W., & Susmiati, S. (2020). The Implementation Of 3S (SDKI, SIKI, SLKI) to The Quality Of Nursing Care Documentation In Hospital’s Inpatient Rooms. STRADA Jurnal Ilmiah Kesehatan, 9(2), 1323–1328. https://doi.org/10.30994/sjik.v9i2.468
Tauran, I., & Tunny, H. (2023). Preparation of Nursing Care Standards and Nursing Care Guidelines as Standards for Implementing Nursing Care Based on SDKI, SLKI and SIKI at Class II Hospital Prof. Dr. J.A. Latumeten Ambon. Jurnal Mahasiswa Ilmu Farmasi Dan Kesehatan, Vol.1(3), 249–256. https://doi.org/10.52395/ujpkm.v2i1.277
Wahyuliati, T. (2024). Efektifitas Pelatihan 3S (SDKI,SLKI,SIKI) pada Perawat Pelaksana terhadap Kesesuaian Pendokumentasian Asuhan Keperawatan. JPPNI, 09(02), 2–11. https://doi.org/DOI:http://dx.doi.org/10.32419/jppni.v9i2.579
WHO. (2022). World Health Statistics 2022 (Monitoring health of the SDGs). https://doi.org/https://www.who.int/data/gho/publications/world-health-statistics
Widyastuti, Y. (2024). Training of SDKI SLKI SIKI Application at PKU Muhammadiyah Hospital, Karanganyar. Jurnal Pengabdian Dan Keberlanjutan Masyarakat, 01(01), 12. https://doi.org/https://doi.org/10.62383/bersama.v1i1.1268
Wisuda, A. C. (2020). Performance of Implementing Nurses in Documenting Nursing Care in Inpatient Installations. Jurnal ’Aisyiyah Medika, 4, 230–238. https://doi.org/10.36729/jam.v4i2.223
Wisuda, A. C., & Suraya, C. (2024). Implementation of 3S (SDKI, SLKI, SIKI) in Nursing Services in Inpatient Rooms. Ukhuwah?: Jurnal Pengabdian Kepada Masyarakat, 2(1), 45–53. https://doi.org/10.52395/ujpkm.v2i1.427
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Aris Citra Wisuda, Citra Suraya, Miming Oxyandi, Isrizal

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.






.png)





